The Clinical Event
The benefits of an event-driven digital system to clinical care
Written by: Frank O’Connor, Cloud and Solutions Architect and member of the Innovation team at IMS MAXIMS
“One of the great challenges in healthcare technology is that medicine is at once an enormous business and an exquisitely human endeavour; it requires the ruthless efficiency of the modern manufacturing plant and the gentle hand-holding of the parish priest; it is about science, but also about art; it is eminently quantifiable and yet stubbornly not.”
The history of progress is the history of problems being solved. Any solution, however, risks introducing new problems. Digitisation introduces automation, standardisation and efficiency into health record collection. At the same time, however, it has led to clinician complaints about:
Increased workforce pressures
Prevalence of medical errors
Extra clinical hours spent on administrative tasks
A need to address increasingly complex services
Inaccurate or incomplete conversations or pathways with patients
It seems that something in Wachter’s disjunction between science and art may be at play here, but if so, what is the precise nature of that disjunction and how did it arise? This is a broad and complex issue, but we can examine some pertinent areas of it by looking at the patterns arising across innovative shifts made in the history of health record collection.
Pen and Paper
The original health record was a physically recorded file. In many cases, it still is.
The physical record solves the basic problem of correctly remembering and recalling patient history. It also introduces new problems. These include inconsistency in recording content and style, a large degree of space usage, time consumption and difficulties in cross-referencing.
The introduction of forms and process into paperwork went some way to solving the problem of inconsistency in recording but problems of storage space, time-use and cross-referencing remain.
Digital
Digitisation is intended to solve or mitigate some of the extant problems of pen and paper, such as difficulties in cross-referencing and use of storage space. Because digital data can be centrally stored in relational databases, it is easy and quick to cross-reference. Physical file storage is also freed up.
The problem that digitisation does not solve, however, is the amount of time needed to enter data. The ideas of process and the form are kept. The difference is that clinicians enter information into an on-screen form.
The Problem with Forms
Of course, there is no such thing as the typical health care worker, but we can put a lens on the issue by looking at the notion of emergencies in a busy hospital.
A hospital clinician, throughout their day, may witness clinical events at different times, with different patients and in different locations. Each event will have its own degree of urgency.
Juggling these events, focusing on patients and moving from location to location are all processes antithetical to entering information into a form. The former require agility in motion, concentration, analysis and sympathy. The latter requires consistency in attention, stillness and recall.
This disjunction parallels Wachter’s characterisation of the difference between science and art in healthcare. The form is on the side of science, automation, consistency and time. The clinical event is on the side of art, the human, speed and adaptation.
The problem applies even if, as in many cases, the job of form filling is passed on to dedicated data entry specialists, who work from the day’s records to update the system overnight. In addition to cost issues, the disjunction between the two scenarios risks introducing errors and omissions.
Event-Driven Systems
To solve this problem, we may consider moving the locus of record-keeping away from form-filling, which was inherited from pen and paper, and placing it instead on the event.
Clinical environments can be viewed as systems developed for processing healthcare events, such as the accident, the developing symptom or the drop in test result values. Some of these may be predictable and some not. Some may be critical and others benign.
If we can harness these events and use them to drive digital care and record collection, then we can reduce the disjunction between the event and the record entry. That gets us closer to a system that saves time, provides real-time decision support and automatically collects data throughout the working day.
What might an event-driven clinical system look like? In the first place, it should mirror the characteristics of clinical events. It needs, consequently, to be:
Distributed, in the way that events are, across locations
Made up of many discreet, but connected elements - since events themselves are also discreet and connected
Organised into flows. An efficient event-driven system needs to replicate the way that some specific events trigger other ones
Work in real-time, just as events do
In addition to these mirroring characteristics, a good event-driven system should also achieve three further objectives:
It needs to be integrated with current clinical systems to optimally record events
It should record all relevant event data as it occurs (saving clinicians time and effort in filling in forms)
It should notify, guide, and provide real-time decision support to clinicians – in effect becoming the invisible guiding hand that frees them up to focus further on patients.
How to build an Event-Driven System
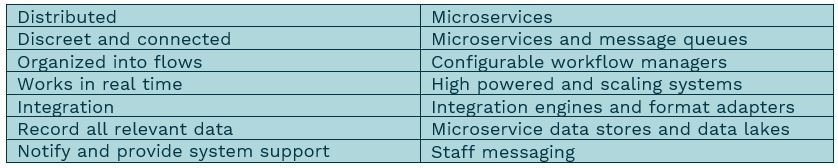
So much for the theory of an event-driven system. How can we create one in reality? If we return to the characteristics listed above, we see that each can be mapped onto an already extant architectural feature or application, as follows:
This provides us with a mapping from theory to reality. The final step would be making that reality concrete. We have achieved that goal over the last two years at IMS MAXIMS.
The SMART Platform
The SMART Platform is a portable, distributed, event-driven, patient-centered healthcare system that is designed to leverage events in a way that removes barriers to patient care.
SMART integrates with clinical devices and the Internet of Things to enable care across systems and domains and to give patients more ownership of their own care.
Distributed workflows, messaging and the decision process can be enhanced with AI, enabling the individual clinician to focus more and better on patient interaction.
In addition to real-time event enhancement, the SMART platform works in combination with our Maxims EPR for seamless integration with administrative and clinical functions, opening the possibility for an enterprise-wide approach to population health management. SMART can derive actionable information at the EPR level and ensure that it is aggregated, harmonized and centralized for easy retrieval.
The platform runs in real time on any cloud-based or on-premise infrastructure, has a small footprint and can be integrated with the majority of FHIR, HL7 and messaging systems.
We see SMART as the next step, a clinical event in the harnessing of clinical events. SMART’s event driven engine addresses some of the most pressing challenges experienced in healthcare today. It enables users to leverage healthcare data and to naturally fit with administrative and clinical workflows. SMART interactions work best for patients and healthcare professionals, offering a personalised experience to patients whilst giving valuable time back to hospital staff.